July 2025

From Freezer to Failure? The Hidden Risks of Cryopreservation in Cell Therapy
Written by: Robin Sieg & Prof. Dr. Kathrin Adlkofer
In the development and application of cell-based therapies, the choice of a suitable transport and storage strategy plays a central role. Over the past years, cryopreservation has evolved into the gold standard for practical and historically established reasons. At the same time, evidence is mounting that especially for short-term transport of cell products, there are more arguments against this approach than in favor. Cryopreservation can lead to substantial losses in cell viability and functionality and is often associated with toxic additives and laborious thawing protocols.¹ Despite these known limitations, freezing remains established practice in many settings. This article highlights the challenges and limitations of cryopreservation in clinical contexts and discusses sound alternatives for the timely and function-preserving transport of living cell products.
Cell therapeutics, whether autologous or allogeneic, are among the most sensitive and complex biologics in modern medicine. Their efficacy depends not only on the survival of the cells but significantly on their functionality within the target tissue. In this context, cryopreservation represents a compromise: although it has become established, cryopreservation is increasingly being viewed critically.
Originally introduced for practical purposes, there are now more arguments against it than for the method, particularly for short and mid-term transport, ranging from functional impairments to toxicological concerns and complex procedural steps. In light of growing evidence about post-thaw functional loss and regulatory hurdles when modifying processes retrospectively, a rethinking is necessary. The focus is therefore shifting toward actively controlled transport systems as a potential alternative, especially for fresh cell products with high functional sensitivity.

Cryopreservation has earned its firm place in bioproduction for good reason. It offers flexibility in planning, allows for long-term storage, and supports batch production of cell products². However, the freezing and thawing process triggers a cascade of physiological stress factors. Ice crystals form during freezing, which can mechanically damage cell membranes³. At the same time, the phase transition leads to a local increase in the concentration of dissolved substances in the remaining liquid fraction, causing osmotic shifts. - Salt ions migrate into the still-unfrozen cell compartments, which can lead to massive osmotic pressure⁴.
These effects severely impair cell structure and increase the risk of irreversible damage. In addition, there is selective pressure on certain cell populations: particularly functionally active and sensitive cells, which are often clinically critical, are typically more vulnerable to cold stress⁵. This can result in more robust, but possibly less functional, cell fractions dominating after thawing. The resulting cell population may therefore not reflect the original therapeutic intent. The use of cryoprotectants such as DMSO, which is intended to mitigate these effects, brings with it its own toxicological challenges, both for the cells and the patients⁶. Studies consistently show that the viability of therapeutic cells after thawing often decreases significantly, with values sometimes falling below 70%⁷.
But survival alone is not enough. Even if the cells survive the process, their functionality often declines. For example, natural killer (NK) cells show reduced cytotoxic activity after thawing⁸, and mesenchymal stem cells (MSCs) reduce cell viability and increase apoptosis level⁹, which can impair therapeutic efficacy. It is a dangerous misconception to equate cell viability with cell functionality. In the context of cell therapy, mere survival is not sufficient, cells must be capable of targeted action, engraftment, proliferation, and the execution of specific biological functions.
Human pluripotent stem cells (hPSCs), including induced pluripotent stem cells (iPSCs), are highly sensitive to environmental stressors such as cryopreservation as well. While current slow-freezing protocols may support acceptable post-thaw viability, they are often associated with spontaneous differentiation or phenotypic alterations. These subtle but critical changes can compromise the therapeutic integrity of the cell product, resulting in a cell population that no longer reflects the intended function or identity¹⁰. These functional impairments often remain undetected in standard viability tests, creating a dangerous false sense of security.
For Advanced Therapy Medicinal Products (ATMPs), especially in early clinical phases, product integrity from lab to bedside is critical. Nevertheless, logistics are often treated as a secondary issue. During development, the focus typically lies on upstream processes and manufacturing, while transport is only addressed shortly before clinical implementation. This oversight can have serious consequences. Once an IND (Investigational New Drug) dossier is submitted and approved, the transport method is fixed. Retrospectively switching from cryopreservation to fresh transport requires additional validation, regulatory amendments, and potentially new comparability studies, a time- and resource-intensive process that can delay patient access to innovative therapies and the product’s market entry.
It is therefore strongly recommended to evaluate transport methods early in the development phase, especially for fresh cell products. Validating controlled, non-freezing transport systems reduces the risk of later modifications and better aligns with growing regulatory requirements and clinical expectations.
The comparison between cryopreservation and actively controlled live-cell transport is by no means theoretical, it becomes apparent across many dimensions:
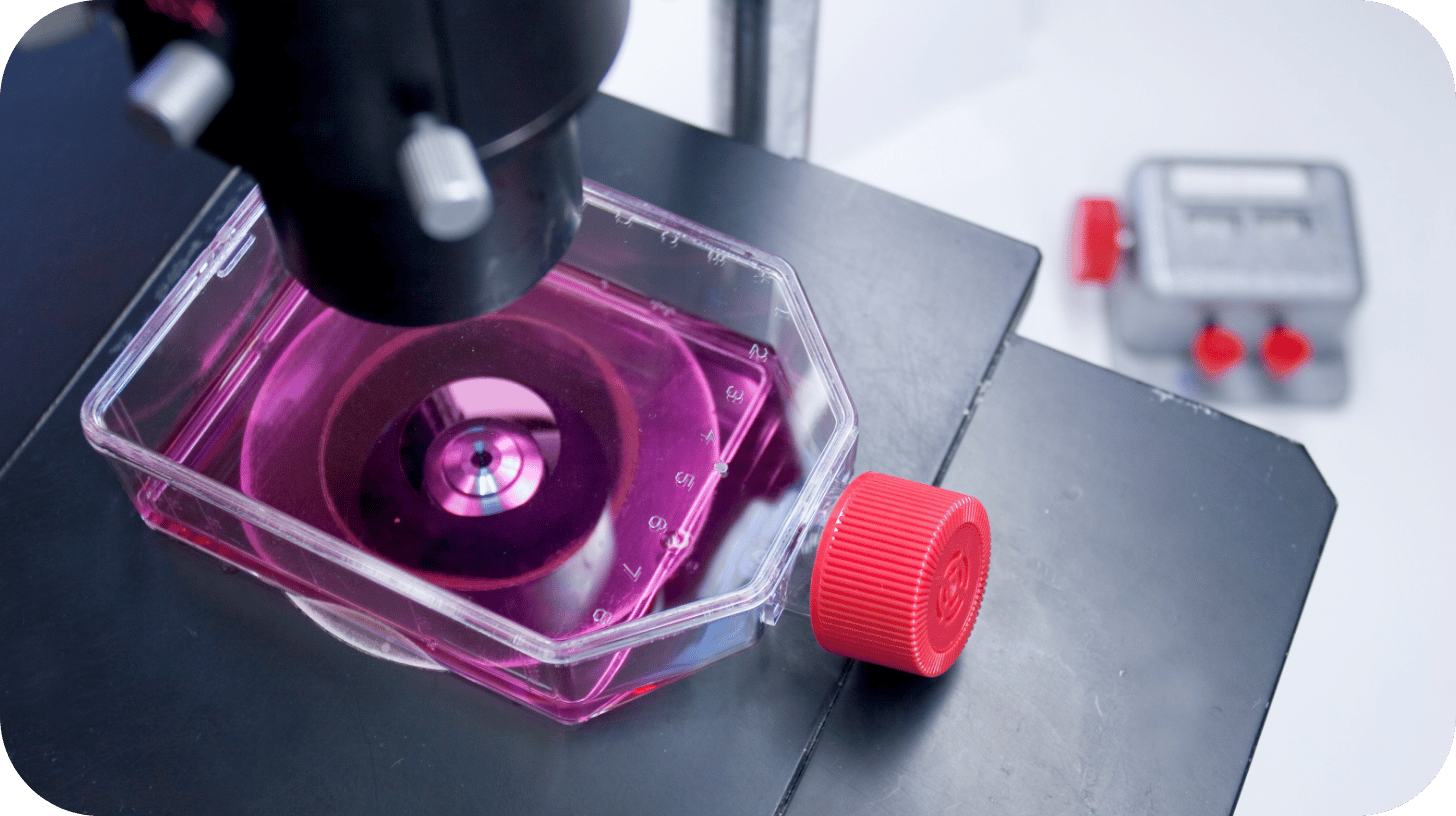
In an active transport system like Cellbox™, cells remain under physiological culture conditions throughout. No injuries occur from freezing, thawing, or temperature fluctuations. Cells are therefore protected from osmotic and mechanical stress, and no metabolically active cryoprotectants such as DMSO are needed. Particularly sensitive cell types, cell structures, or constructs retain their structure, function, and morphology thanks to a controlled CO₂ atmosphere and precise temperature regulation (e.g., at 37 °C). There are no pH shifts or exposure to toxic buffering systems. In addition, the environmental conditions in an active transport system like Cellbox™ are continuously recorded via data logging. These data enable retrospective quality analysis and provide regulatorily relevant documentation, a key advantage over conventional transport solutions without monitoring.
In contrast, cryopreservation disrupts nearly all of these parameters. Cells are exposed to thermal and osmotic stress, toxic additives are introduced, and multiple processing steps are required at the destination: thawing, washing, seeding. This increases variability, prolongs process duration, and compromises reproducibility. In multicenter studies, this can become a serious challenge.
These differences become particularly apparent when comparing logistical requirements. Cryo transport requires cold-chain infrastructure, dry ice or liquid nitrogen, thawing protocols, and trained personnel. Delays or environmental factors can cause irreversible damage. Active live-cell transport systems, on the other hand, function like mobile incubators. They maintain stable conditions even during long-distance transport, ideal for decentralized production or multicenter studies. And the impact goes further: a cell product that arrives ready to use saves clinical staff valuable time and reduces potential sources of error. No thawing. No washing. No waiting. Science and therapy without interruption or compromise.
The crucial question is therefore: Is freezing still justified in your process? Or is it time to choose a strategy that reflects the value and complexity of your product?

